 Proper Needle Selection for Blood Collection : September 2019 - MedicalLab Management Magazine
Proper Needle Selection for Blood Collection : September 2019 - MedicalLab Management MagazineHypodermal needle This article needs additional appointments for . Please help. Unsolicited material can be challenged and disposed of. Finding sources: – · · · · (August 2010) () you need additional citations for ····A hypodermic needle (from πο- (hypo- = below), and δ Conceptρμα (derma = skin), one of a category of medical tools that enter the skin, called sharp, is a very thin and hollow tube with a sharp tip. It is commonly used with a , a hand-operated device with a piston, to substances in the body (e.g., solutions that contain several drugs or liquids) or extract fluids from the body (e.g. blood). High body hypodermic intervention is particularly useful in loss of catastrophic blood or treatment. hypodermal needles A hypodermal needle is used for quick delivery of liquids, or when the injected substance cannot be ingested, either because it would not be (like with ), or because it would damage the . It is also useful to deliver certain medicines that cannot be delivered orally due to vomiting. There are many possible for an injection, with (in one ) and (in one ) is the most common. Hypodermal needle also serves an important role in research environments where sterile conditions are required. Hypodermal needle significantly reduces contamination during a sterile. The hypodermal needle reduces contamination for two reasons: First, its surface is extremely smooth, which prevents the air from being trapped between irregularities on the surface of the needle, which would later be transferred to the media (e.g.) as contaminants; secondly, the surface of the needle is extremely acute, which significantly reduces the diameter of the remaining hole after drilling the hole and therefore prevents the larger microbes from being contaminated. ContentHistory[]Use and early experimentation[] ]The ancient Greeks and Romans knew the injection as a method of medicinal delivery of the observations of the sheds and poisoned weapons. There are also references to "anunizar" and "innotion" in the Old Testament, as well as Homer's works, but injection as a legitimate medical tool was not really explored until the seventeenth century. performed the first confirmed experiments with raw hypodermal needles, performing intravenous injection in dogs in 1656. These experiments consisted of the use of animal bladders (such as syringe) and goose quills (such as needle) to administer drugs such as opio in intravenous form to dogs. Wren's main interest and others was to learn whether traditionally administered drugs would be effective intravenosely. In the 1660s, J. D. Major of Kiel and J. S. Elsholtz of Berlin were the first to experiment with injections in humans. These early experiments were generally ineffective and in some cases fatal. The injection fell from the favor for two centuries. Development of the nineteenth century[] The nineteenth century saw the development of effective medicines in small doses, such as opiates and estricnine. This encouraged renewed interest in the direct and controlled application of medicine. "Some controversy surrounds the issue of priority in hypodermic medication."It is generally credited with the first successful injection in 1844. 's main contribution was the all-glass syringe in 1851, which allowed the user to estimate the dose based on the fluid levels observed through the glass. The wood used hypodermal and syringe needles mainly for the application of localized and subcutaneous injection (localized anaesthesia) and was therefore not so interested in precise doses. Simultaneous to Wood's work in Edinburgh, of Lyon also experimented with sub-dermal injections in cattle using a syringe of his own design. Pravaz designed a 3 cm (1.18 inches) long and 5 mm (0.2 inches) in diameter; it was made entirely of silver. , a surgeon from London, is credited with the coinage of the term "hypotermic" to describe subcutaneous injection in 1858. The name originates from two Greek words: hypo, "low", and derma, "skin". In addition, Hunter is accredited with the recognition of the systemic effects of the injection after noting that a patient's pain was relieved regardless of the proximity of the injection to the pained area. Hunter and Wood were involved in a long dispute over not only the origin of the modern hypodermic needle, but also because of their disagreement with the effect of the medication once administered. Modern improvements[]Dr. Wood can be attributed largely to the popularization and acceptance of injection as a medical technique, as well as the widespread use and acceptance of the hypodermal needle. The basic technology of the hypodermal needle has been largely unchanged since the nineteenth century, but as the years progressed and the medical and chemical knowledge improved, small improvements have been made to increase safety and effectiveness, with needles being designed and adapted for very particular uses. The needle specification trend for use began in the twenties, especially for the administration of insulin to diabetics. The beginning of the Second World War stimulated the early development of partially disposable syringes for the administration of morphine and penicillin in the battlefield. The development of the hypodermal needle was stimulated in the 1950s for several reasons. The Korean War created blood shortages and in response sterile syringes were developed to collect blood. The widespread immunization of poliomyelitis during the period requires the development of a completely disposable syringe system. The 1950s also saw the increase and recognition of the cross contamination of the needles used. This led to the development of the first fully disposable plastic syringe by New Zealander Colin Murdoch in 1956. This period also marked a change in the interest of the needle specifications to general sterility and safety. In the 1980s, the increase in the HIV epidemic was observed and concern for the safety of cross-contamination of the needles used was renewed. New safety controls were designed on disposable needles to ensure the safety of medical workers in particular. These controls were implemented in the needles themselves, such as retractable needles, but also in the handling of used needles, especially in the use of hard surface removal receptacles found in each medical office today. By 2008, the needles of all kinds were in production and in limited use. One version was recorded from 1.2 mm in the center to 0.72 mm in the tip (a needle equivalent to 22 metal calibers), with a 70% ID/OD ratio. Manufacture[ ] Power needles are usually made from a tube through a process known as where the tube is progressively smaller through to make the needle. The end of the needle is to create a pointed tip, allowing the needle to easily penetrate into the skin. Gauge[]The main system to measure the diameter of a hypodermic needle is the (also known as the Stubs Iron Wire Gauge); it is mainly used for catheters. There are several needle lengths available for any given meter. Common medical needles vary from 7 meters (the largest) to 33 (the smallest). The 21-caliber needles are more commonly used to draw blood for test purposes, and the 16- or 17-caliber needles are more commonly used for blood donation, as the resulting lower pressure is less harmful to the red blood cells (also allows more blood to be collected in a shorter time). Although reusable needles remain useful for some scientific applications, disposable needles are much more common in medicine. Disposable needles are embedded in a plastic or aluminium concentrateer that attaches to the syringe barrel by a pressure or torsion adjustment. These are sometimes referred to as "Luer Lock" connections, referring to the brand. The male and female lock and concentrater, produced by the manufacturers of pharmaceutical equipment, are two of the most critical parts of disposable hypodermic needles. Use by non-specialists[ ] Power needles are usually used by medical professionals (, , , , , , , ), but are sometimes used by patients themselves. This is more common with , which may require several injections a day. It also occurs with patients who have or other serious patients. Such patients may need to take injections or may need to take injectable medications to use for first aid in case of severe allergic reaction. In the latter case, these patients usually wear a syringe (e.g.) (e.g., ), or . Rapid injection of one of these medications may stop a severe allergic reaction. Patients can also be treated by injection; several MS therapies, including various preparations, are designed to be self-administered by subcutaneous or intramuscular injection. In some countries, patients may be prescribed in injectable form, which is injected directly into the base or side of the penis with a very fine hypodermic needle. Hypo-powerful needles are also used by untrained users (e.g. injection and water solutions). Before governments reached current levels of awareness of the spread of diseases through shared needles, hypodermal syringes in many countries were only available by statute. Thus, to limit the spread of shared injection equipment, for example, many countries have in most of the largest cities. In some countries, these programmes are totally or partially subsidized by the government. Depleted needles, manufactured without a sharp and generally non-sterile bezel, are industrially used to fill small containers or accurately apply small amounts of solvent or glue. Phobia[] It is estimated that anywhere from almost 3.5 to 10 per cent of the world ' s population may have one needle (tripnophobia), and it is much more common in children from 5 to 17 years of age. Topical anesthetics can be used to desensitize the area where the injection will take place to reduce pain and discomfort. For children various techniques can be effective in reducing needle-related discomfort or pain. The techniques include: distraction, , combined and breathing techniques. See also[]References[]148552880abcabc3430abcab10External links[] Wikimedia Commons has media related to . ##### ##################################################################################################################################################################################################################################################### (), 00 , (IUD) () solution system (in the tissue/blood) , () (), 00 00 , Navigation menu Personal tools Named spaces Variants Views More Search Navigation Contributed Tools Printing/exporting Other projects Languages
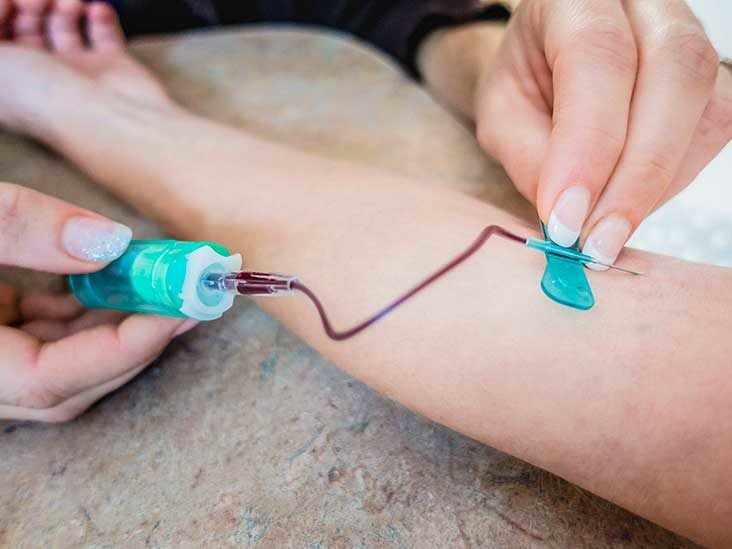
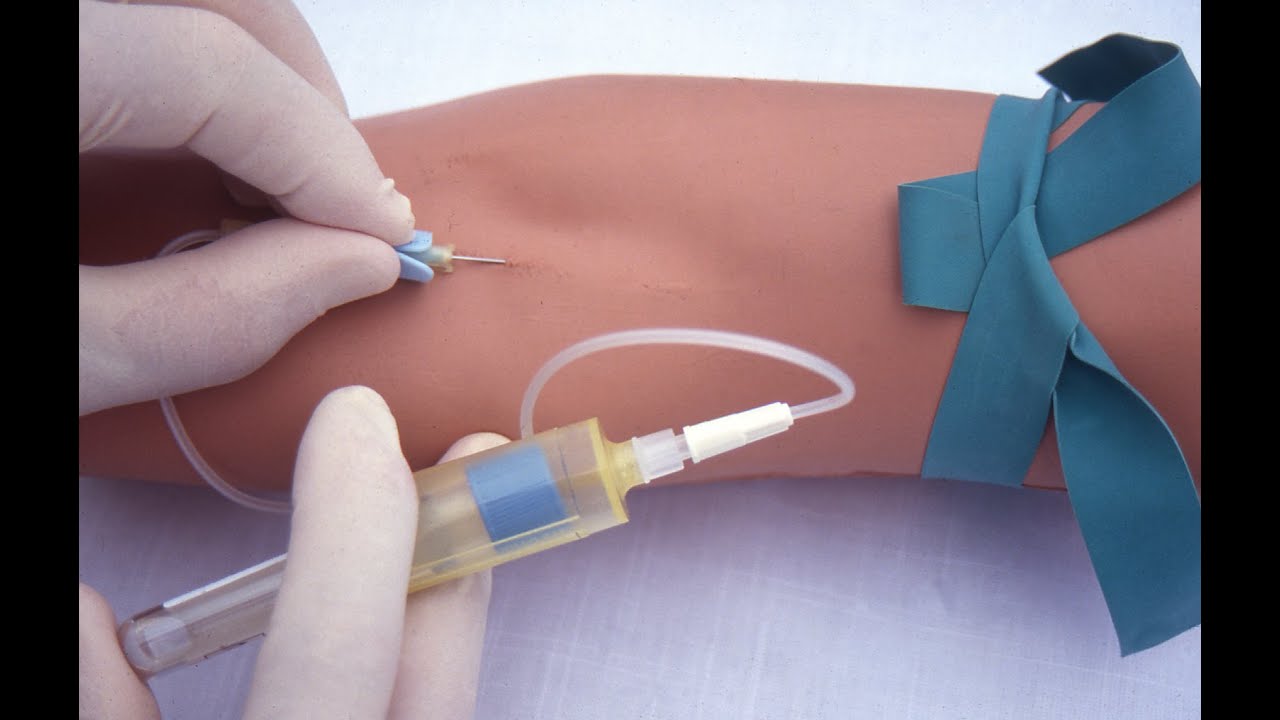
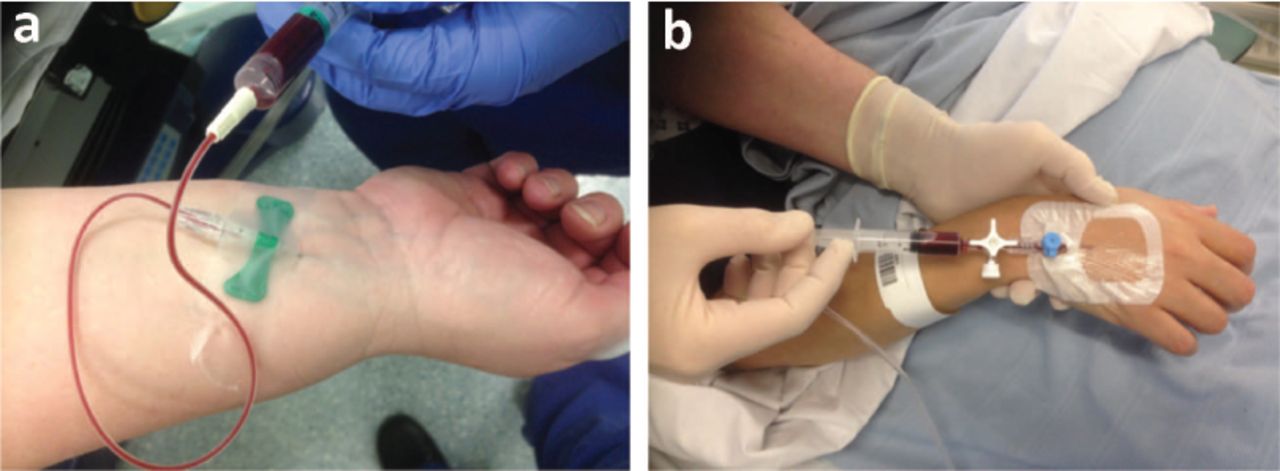
All on the butterfly needles These can be useful for blood drawings and to offer IV Therapies Michael Menna, DO, is a certified and active emergency medicine doctor in White Plains Hospital, New York. A butterfly needle is a device used to extract blood from a vein or deliver intravenous therapy (IV) to a vein. It is also called a scalp infusion set or scalp vein set, a butterfly needle consists of a very thin hypodermic needle, two flexible "alas", a flexible transparent tube and a connector. The connector can be attached to a vacuum tube or collection bag to extract blood or tubes from a IV bag to deliver liquids or medications. Medicines can also be sent directly to the connector through a syringe. Butterfly needles offer certain advantages over straight needles. For example, they allow more precise placement, especially in the veins difficult to reach. They are not the best choice in each case, however. Mistaken identity At first glance, a butterfly needle resembles one, which is also flatbed. However, the hub needles are folded at a 90-degree angle so they can safely be placed in an implant. For which butterfly needles are used Phytotomists regularly use butterfly needles to get blood samples for (CBC), , , , and other blood-based tests. These needles are also commonly used in blood banks for people who want to donate blood. Butterfly needles can also be used to deliver intravenous fluids if you are dehydrated and cannot drink liquids or cannot drink enough to compensate for fluid loss. They are also useful for the delivery of medicines (such as ) directly in a vein or little by little infusing IV therapies (such as or ) intravenous. Although butterfly needles can be left in a vein for five to seven days if properly insured, they are more commonly used for short-term infusions. Regular or continuous infusions usually access through a larger vein through a line or (PICC). Types Although all butterfly needles are similarly designed, there are variations. Butterfly needles are measured in calibers and usually vary in size from 18 calibers to 27 calibers. The higher the caliber, the smaller the needle. As an illustration, a needle of 27 calibers is the size commonly used for . Smaller caliber needles are used if an injectable fluid is thick or if blood is collected for transfusion. Most butterfly needles are no more than three quarters of an inch (19 millimeters). The IV or collection container is attached to the pipe that is connected to the needle, instead of the needle. This is useful, as there is less chance of injury if yanked or dropped. The tube can range from 8 inches to 15 inches (20 to 35 centimeters). The shortest tubes are used for blood drawers. The longer ones are intended for IV applications and can have roller valves to regulate the flow. Tubes can also be colored so that nurses can differentiate which line is the one that is used more than one. Some butterfly needle connectors have built-in "man" ports that can be inserted into vacuum tubes. Other connectors have "women" ports in which syringes or lines can be inserted. How Butterfly Needles Are Used During the venipuncture (the insertion of a needle into a vein), one or nurse will keep the butterfly needle by its wings between the thumb and the index finger. Because the hypodermic needle is short and the grip is close to the needle, the butterfly needle can be placed more accurately than a straight needle, which can often roll or move your fingers. The short and thin needle is inserted into a vein at a shallow angle. Once inserted, the venous pressure forces a small amount of blood in the transparent tube, providing confirmation that the needle is properly placed. Wings can also serve to stabilize the needle once it is in place, preventing it from surrounding or changing. Once used (blood is removed or the medication is delivered), the whole unit is thrown into a sharpener removal container. The puncture wound is sold. Advantages Due to its small size (much smaller than a ) and shallow-angle design, butterfly needles can access surface veins near the surface of the skin. This not only makes them less painful to use, but allows them to access small or narrow veins, such as babies or the elderly. Butterfly needles are ideal for people with small or stunts veins and can even be inserted into the small veins of the hand, foot, heel or scalp. Butterfly needles are ideal for people who are hesitating on needles because they are less threatening. They are also less likely to cause profuse bleeding, nervous injury, or a vena collapse once the needle is removed. The most recent models have a slide and block case that is automatically slided over the needle, as it is removed from a vein, preventing and reusing a needle used. If you have been told that you have small veins and have had defiant blood drawings in the past, you might consider requesting the use of a butterfly needle. Disadvantages That said, butterfly needles are not for everyone. Due to its small needle size, blood collection tends to be slower. This can be problematic in a blood bank if a person is squamous or in urgent situations where the blood is needed quickly. In situations like these, the needle size selection is key. Even for a routine drawing of blood, the incorrect needle size can result in blocking and the need for a second draw if a lot of blood is needed. Because a needle is left in the arm instead of a catheter or for the purpose of an infusion, a butterfly needle can damage a vein if the unit is suddenly torn. Even if the right size needle is used, the needle can be blocked during the treatment if it is not placed properly. As a thumb rule, butterfly needles should only be used for infusions IV of five hours or less. Sign up for our newsletter Health Tip of the Day and receive daily advice that will help you live your healthiest life. Thank you, for signing. There was a mistake. Please try again.. In: Sedation. 6th edition. 2018:308-318. doi:10.1016/b978-0-323-40053-4,00024-xOhnishi H, Watanabe M, Watanabe T. . Arch Pathol Lab Med. 2012;136(4):352. doi:10.5858/arp.2011-0431-LEIalongo, C. and Bernardini, S. Biochem Med (Zagreb). 2016 Feb 15;26(1):17-33. DOI: 10.11613/BM.2016.002.Wolowitz, A.; Bijur, P.; Esses, D. et al. Society for Academic Emergency Medicine Annual Meeting; Atlanta, Georgia; May 2013. DOI: 10.1111/acem.12245. Thank you, for signing. There was a mistake. Please try again.

Hypodermic needle - Wikipedia
needle gauges | Nurse, Nursing school, Nursing school survival:max_bytes(150000):strip_icc()/butterfly-needles-for-blood-draws-and-simple-ivs-430065-color-V1-68cec23a52564677bb7989c29a8e81d0.png)
Butterfly Needles: Pros and Cons for Blood Draws and IVs
Common Gauges of Needles Used for Venipuncture | PhlebotomyU
Needle gauge comparison chart | Phlebotomy, Medical assistant, Nurse
Venipuncture - Wikipedia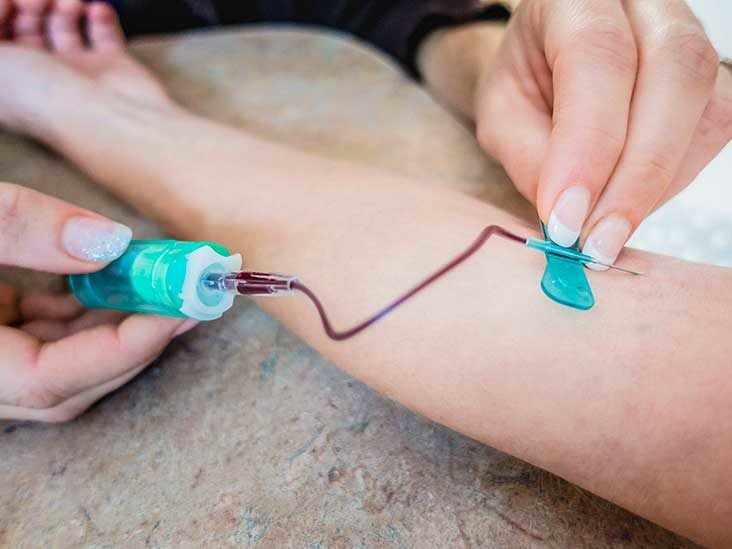
Butterfly Needle for Blood Draw: How It Works and Why It's Used:max_bytes(150000):strip_icc()/how-to-select-the-correct-needle-size-for-an-injection-2616536-FINAL-f42600395a324d71b8b3fc4f13f5723d.png)
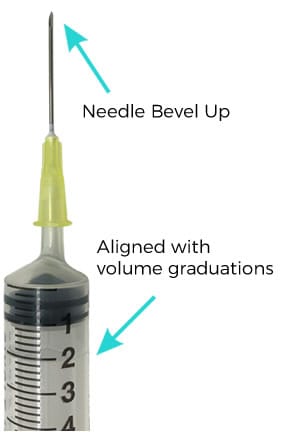
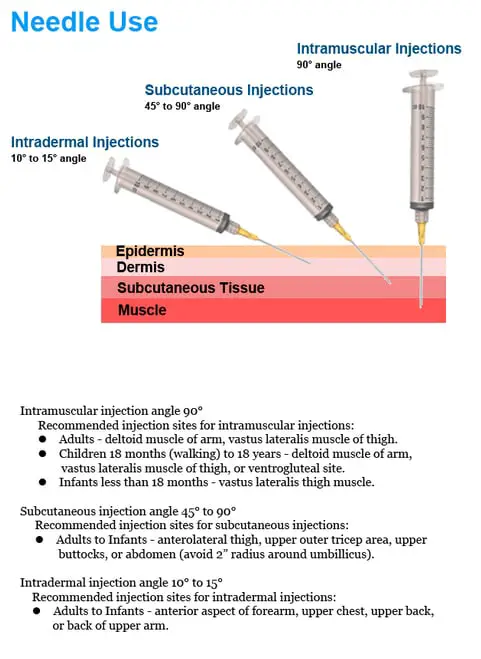
Choosing a Syringe and Needle Size for an Injection
BD Vacutainer Eclipse Blood Collection Needle - BD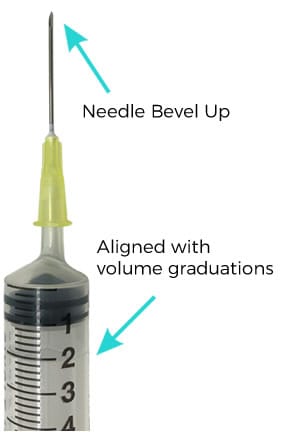
Jugular Venepuncture - Get the best sample with these tips for VNs | Australian College of Veterinary Nursing
Use Of Hypodermic Needle Or Medical Needle Are Less Pain-Full
How to Draw Blood from Cattle • The Prairie Homestead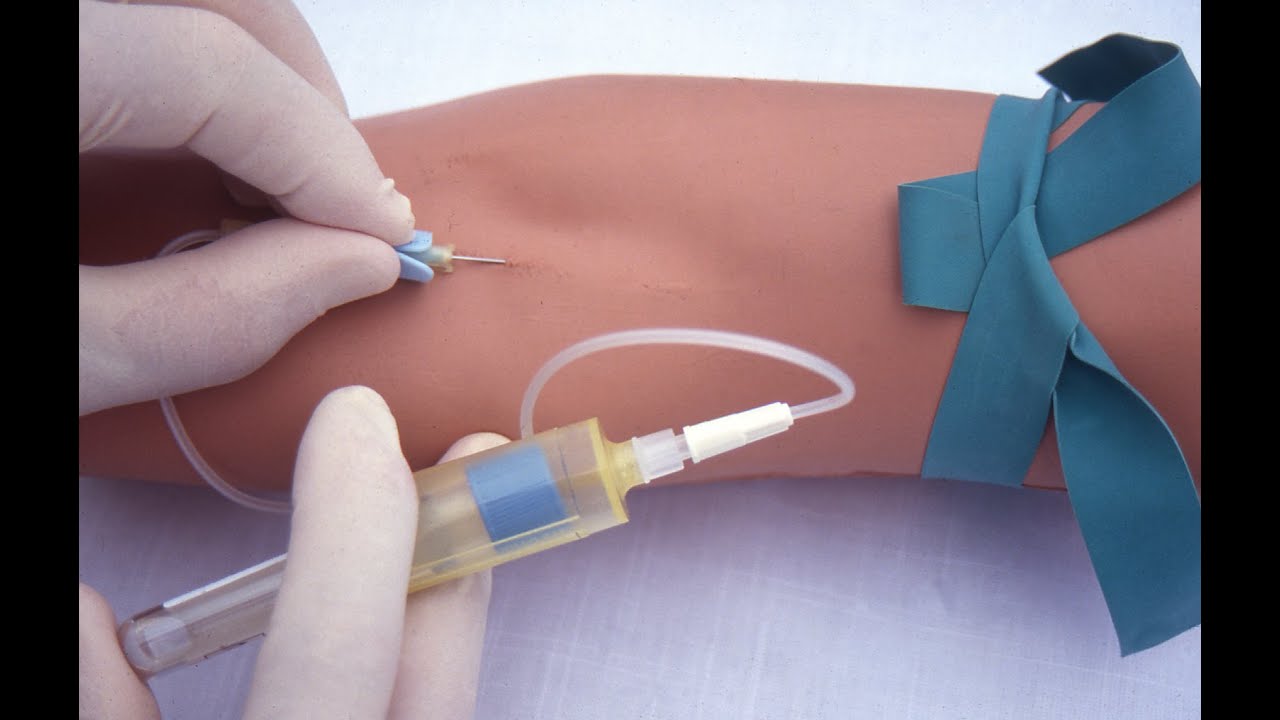
Performing a venipuncture using a butterfly needle - YouTube
Why could the phlebotomist only get 2ml of blood from my vein in my hand in 5 mins? - Quora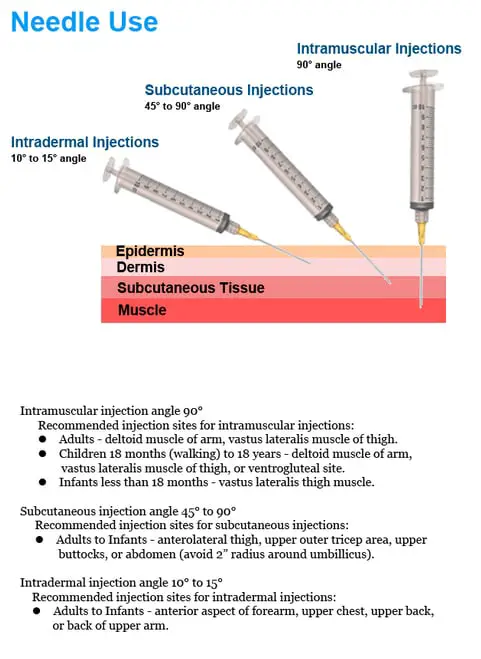
Syringe and Needle Sizes - How to choose (Guide) | LaboratoryInfo.com
The right way to draw blood and use needles | Brunet
Butterfly Needle for Blood Draw: How It Works and Why It's Used
Venipuncture - Wikipedia
Top Gun Phlebotomy - Butterfly Use: The Good, the Bad, and the Ugly - Insights
janmarthy
BD Vacutainer® Safety-Lok™ Blood Collection Set - BD
We Asked Nurses and Phlebotomists How to Make Blood Tests Easier | SELF
NKF Singapore - FACT: The needle used for dialysis spans... | Facebook
Goat Injections – Goats
Drawing Blood From Baby Can Be a Harrowing Experience
Techniques for bleeding pigs
Iv Gauge Needles | What are the Differences Between 18, 20, 22, Gauge Needles - YouTube
Butterflies Tied to Lower Hemolysis Rates | MedPage Today
Needles - Clinihealth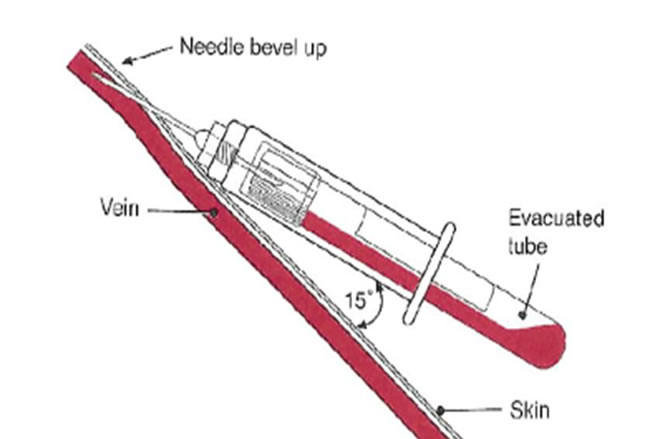
Venipuncture and Arterial Puncture Policy
How to Take Blood Samples from Cattle (with Pictures) - wikiHow
Yellow 30 gauge 12mm (½ inch) needle
Needling the People - Imgur
We Asked Nurses and Phlebotomists How to Make Blood Tests Easier | SELF
Equipment For Drawing Blood/how-to-select-the-correct-needle-size-for-an-injection-2616536-FINAL-f42600395a324d71b8b3fc4f13f5723d.png)
Choosing a Syringe and Needle Size for an Injection
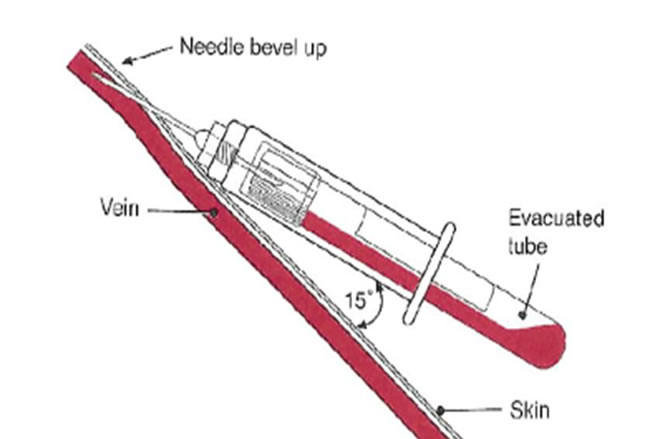
How to undertake venepuncture to obtain venous blood samples
Use Of Hypodermic Needle Or Medical Needle Are Less Pain-Full
Ouch: Challenging Factors During Blood Draws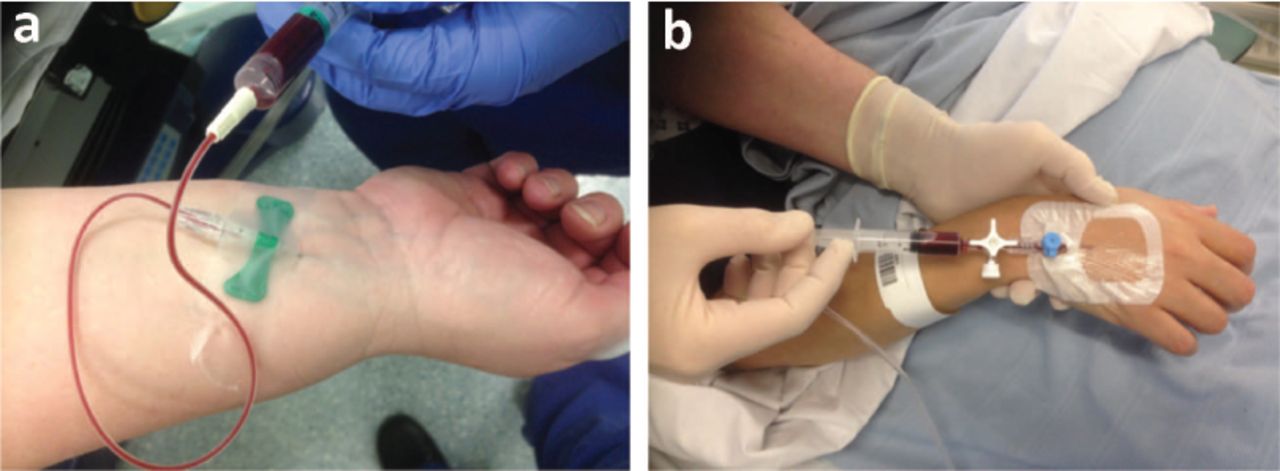
Lessons of the month 1: Learning from Harvey; improving blood-taking by pointing the needle in the right direction | RCP Journals
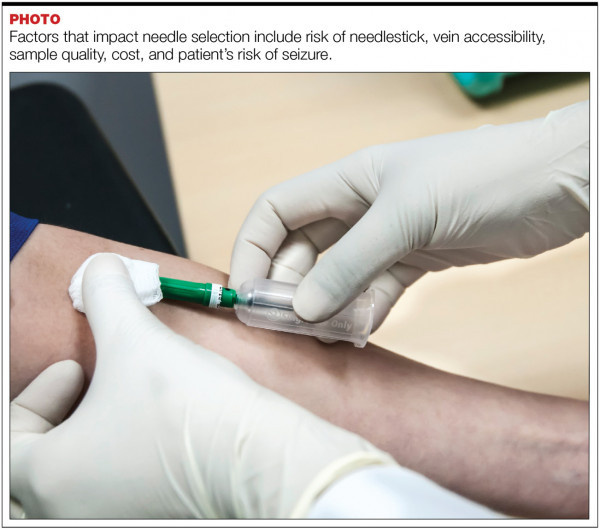
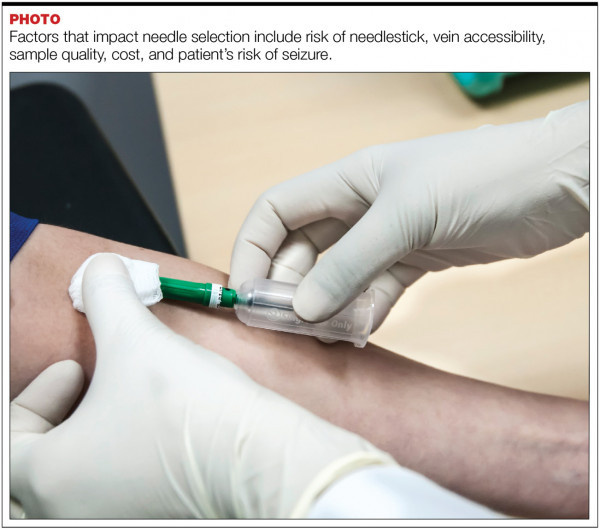 Proper Needle Selection for Blood Collection : September 2019 - MedicalLab Management Magazine
Proper Needle Selection for Blood Collection : September 2019 - MedicalLab Management Magazine

:max_bytes(150000):strip_icc()/butterfly-needles-for-blood-draws-and-simple-ivs-430065-color-V1-68cec23a52564677bb7989c29a8e81d0.png)



:max_bytes(150000):strip_icc()/how-to-select-the-correct-needle-size-for-an-injection-2616536-FINAL-f42600395a324d71b8b3fc4f13f5723d.png)





















/how-to-select-the-correct-needle-size-for-an-injection-2616536-FINAL-f42600395a324d71b8b3fc4f13f5723d.png)



Posting Komentar untuk "what gauge needle is used to draw blood"